Good laboratory practice (GLP) is a set of principles designed to ensure the quality and integrity of data from nonclinical drug safety studies necessary to secure government approval of new drugs, and biological and non-pharmaceutical products.
GLP labs not only ensure ethical treatment of animals but also generate sound evidence of the validity, integrity, and reliability of the nonclinical safety data that regulatory agencies require to approve the use of the product in clinical studies on humans.
The source of GLP requirements in the United States is Food and Drug Administration (FDA) regulations, specifically 21 CFR 21 58, Good Laboratory Practice for Nonclinical Laboratory Studies. The rules come into play during the preapproval phase of FDA regulation when companies must demonstrate product safety and effectiveness on animals before proceeding to clinical trials.
FDA inspectors have the authority to inspect labs, records, and specimens “at reasonable times and in a reasonable manner” to ensure compliance with GLP. If a lab refuses to undergo inspection, the FDA will not include the study in support of the company’s application for premarket approval of the product.
The nine elements of GLP compliance
Here’s an overview of the 9 key elements of GLP regulations and how to comply with each:
1. Staffing and personnel
Maximizing safety and minimizing risk begins with ensuring that nonclinical studies are performed by the appropriate personnel. GLP regulations thus establish rules for personnel. Labs generally need three roles to perform a nonclinical study: i. analysts to perform the work; ii. management to review it; and iii. quality assurance (QA) review. While the analyst and manager can be the same individual, QA must always be an independent person. To comply:
Ensure that all persons involved in and responsible for supervising the study have the necessary education, training, and/or experience to perform their assigned roles
Maintain a current summary of training and experience and job description for each person
Ensure that all personnel wear appropriate clothing and take precautions to avoid contamination of test and control articles and systems
Exclude individuals with an illness that may harm the quality and integrity of the study from direct contact with test systems and test and control articles.
2. Study director
The regulations require a scientist or other professional with appropriate education, training, and/or experience to serve as study director with overall responsibility for its technical performance. Lab management must designate the director before the study begins and replace him/her as necessary thereafter. To comply: the study director must be the single point of control with responsibility for:
Approval of the study protocol and any changes
Accurate recording and verification of all experimental data, including observations of unanticipated responses of the test system
Documentation and correction of unforeseen circumstances that may affect the quality and integrity of the study
Ensuring test systems are as specified in the protocol and that GLP is followed
Transfer of raw data, documentation, protocols, specimens, and final reports to the archives.
3. QA unit
The use of QA processes to minimize product risks is the essence of GLP. Accordingly, the regulations require labs to establish a QA unit responsible for monitoring study compliance with GLP. To comply: ensure the QA unit is separate from and independent of personnel directing and conducting the study and that it exercises the following functions:
Keeping a master schedule sheet of all nonclinical studies conducted at the lab indexed by test article and listing the individual study’s test system, nature, start date, current status, sponsor, and study director
Maintaining copies of all protocols pertaining to studies for which the QA unit is responsible
Inspecting each study at adequate intervals to assure study integrity
Maintaining proper inspection records
Providing written status reports on studies, noting problems identified and corrective actions taken
Ensuring there are no unauthorized deviations from approved protocols or standard operating procedures (SOPs)
Reviewing the final study report to ensure it accurately describes the methods and SOPs.
4. Lab facilities
GLP regulations require that nonclinical studies be carried out in testing facilities of suitable size, design, and construction. To comply: ensure your lab facility has a sufficient number and adequately equipped facilities for all studies, including animal care, storage, and handling of test and control articles, storage of test and control article mixtures, and performance of required routine and specialized procedures.
5. Lab instrumentation and software
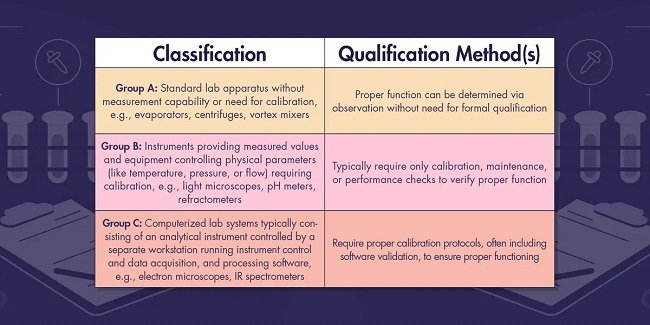
Qualification of the analytical instruments and software used to generate, measure and analyze study data is the heart of GLP. Qualification goes beyond simple calibration, cleaning, maintenance and inspection; it often requires the performance of validation tests to verify that instruments are fit for the intended use and can be relied upon to operate and produce accurate results in accordance with the study protocol. Lab instrumentation is a key target of inspection and the lack of sufficient qualification procedures and documentation is a frequent source of FDA citations and warning letters.
6. SOPs
The GLP regulations establish rules for lab facility operation, including the requirement that written SOPs be implemented for performing nonclinical studies. To comply: at a minimum, be sure you have an SOP for:
Receipt, identification, storage, handling, mixing, and sampling of test and control articles
Test system observations
Lab tests
New method development and validation
Specimen identity and collection
Histopathology
Data integrity, handling, storage, and retrieval
Maintenance and calibration of equipment
If tests involve animals, room preparation animal care, transfer, placement, and identification.
7. Study protocol
Every study must have a written protocol reviewed by the study director that includes a description of the study purpose, experimental design, methods of controlling bias, and information about other essential aspects of the study bearing on product safety and effectiveness.
8. Reporting of results
Labs must prepare a signed and dated final report for each study that includes, among other things:
Information about the sponsor, director, and test facility
Statistical methods used to analyze test data
Test and control articles identified by name, chemical abstracts number or code number, strength, purity, composition, or other appropriate characteristics
A description of all circumstances that may have affected data quality or integrity
Study results, including transformations, calculations, or operations performed on the data, a summary and analysis of the data, and a statement of conclusions drawn from the analysis.
9. Records retention
The final step in GLP compliance is to retain all study documentation records, raw data, and specimens the regulations require you to maintain for whichever of the following periods is the shortest:
Two years from the date of FDA approval of an application for a research or marketing permit based on the study’s results
Five years from the date of submission of the study results in support of such application.
Exception: Studies supporting applications for investigational new drugs (INDs), or investigational device exemptions (IDEs) must be retained for at least five years from the approval date in all cases.
Type and Press enter